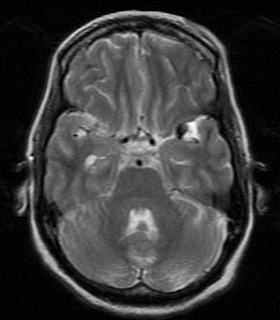
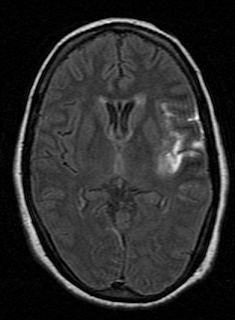
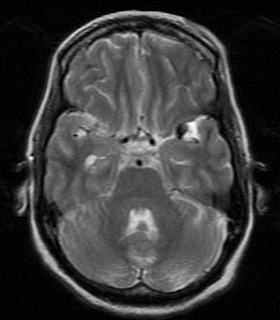
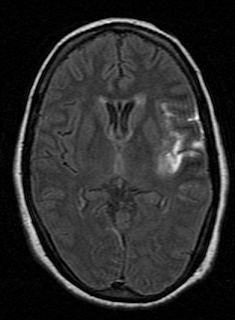
Here is a case of leaking aneurysm for the Radiology Grand Rounds submitted by Dr MGK Murthy of Teleradiology Providers
Concept of the Radiology Grand Rounds is available at- Radiology Grand Rounds.
 The Avenida of 2006 during Mayor Atienza's term?
The Avenida of 2006 during Mayor Atienza's term? Or the Avenida of today (2007) under Mayor Lim?
Or the Avenida of today (2007) under Mayor Lim? Jeepneys once again ply in this portion of Avenida that was previously made into a park during Mayor Atienza's term.
Jeepneys once again ply in this portion of Avenida that was previously made into a park during Mayor Atienza's term. ....and what it was before, a public park with cozy benches and tiled colored flooring...
....and what it was before, a public park with cozy benches and tiled colored flooring...
According to RSNA news Not pitch black, but about 40-25 lux, comparable to a dim hotel room at night, according to one study.
RSNA News May 2007 (p 13-14).
Hat tip--MidEssexRay
 Eurotel Hotel. My favorite hotel in Cubao.
Eurotel Hotel. My favorite hotel in Cubao. New Frontier Theater. Closed for renovation. A place of my vivid romantic memories of yesteryears. I liked the KKK part of this theater. Kataas-taasan, kasuluk-sulukan, at kadilimdiliman.
New Frontier Theater. Closed for renovation. A place of my vivid romantic memories of yesteryears. I liked the KKK part of this theater. Kataas-taasan, kasuluk-sulukan, at kadilimdiliman. Araneta Center Bus Terminal Station
Araneta Center Bus Terminal Station Divisoria Night Market
Divisoria Night Market A Macro shot of Dancing Buddha
A Macro shot of Dancing Buddha A Lion's Head
A Lion's Head