Findings
Figure 1: Sagittal T1 image taken parasagitally at the level of the dentate nucleus. There are T1 hypointensities within the subcortical white matter and in the brachium pontis.
Figure 2: Axial T2 at the level of the cerebral subcortical white matter. There is T2-hyperintensity in the centrum semiovale bilaterally. The signal abnormality is fairly symmetrical.
Figure 3: Axial T2 at the level of the splenium of the corpus callosum. There are T2-hyperintensities within the splenium of the corpus callosum and asymmetrical T2-hyperintensities along the corticospinal tracks within the posterior limbs of internal capsules.
Figure 4: Axial T2 at the level of the middle cerebellar peduncles. There is T2-hyperintensity within the brachium pontis bilaterally. Note that the signal abnormality is symmetrical. Also note that the signal within the pons was normal.
Figure 5: Axial FLAIR at the level of the splenium of the corpus callosum. There are FLAIR-hyperintensities within the splenium of the corpus callosum and asymmetrical FLAIR -hyperintensities along the corticospinal tracks within the posterior limbs of internal capsules.
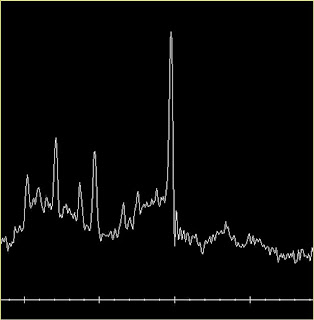
Figure 6 and Figure 7: Axial diffusion weighted and ADC map images at the level of the middle cerebellar peduncles. There is increased signal in both DWI and in the ADC map, consistent with the subacute stage of myelinolysis (four weeks after onset of symptoms). The DWI and ADC maps at the level of the centrum semiovale and splenium (not shown) demonstrated similar findings.
Diagnosis: Extrapontine myelinolysis (osmotic demyelination syndrome)
Central pontine myelinolysis (CPM), was first described in 1959 in patients with a history of alcoholism and malnutrition. Extrapontine myelinolysis (EPM) is the extrapontine manifestation of osmotic myelinolysis and can occur with or without central pontine myelinolysis. In one autopsy series, myelinolysis was found to be confined to the pons (CPM) in about 50% of cases, combined CPM and EPM occurred in about 30 % of cases, and exclusive EPM occurred in about 20% of cases7.
CPM and EPM are characterized by symmetrical loss of myelin with relative preservation of axons and neuronal cell bodies. Pathologically, there is dissolution of the myelin sheaths of fibers. There is however, no evidence of inflammation. The myelinolysis occurs with relative sparing of the nerve cells and axon cylinders.
Although initial reports were largely confined to chronic alcoholics, osmotic myelinolysis has also been seen in patients with electrolyte disturbances, particularly hyponatremia that has been rapidly corrected (more then 10mmol/l/day), and in liver transplant patients being immune-suppressed with cyclosporine. Alcohol continues to be a particularly frequent etiology (up to 40% of cases)7.
Osmotic myelinolysis can affect a variety of sites resulting in a variety of symptoms. The MRI appearance is characteristic with lesions being symmetrical. However, the timing of the appearance of lesions on MRI may be significantly delayed. If there is a strong clinical suspicion of the diagnosis, repeat imaging at 1 to 2 weeks may reveal lesions that were not initially apparent. Diffusion weighted imaging (DWI) might have the capability of detecting lesions undetectable on conventional MRI earlier, with one case report in the literature showing an altered DWI in a patient within 24 hours of symptoms at a time when conventional MRI findings were inconspicuous.
The prognosis of the osmotic demyelination syndrome is variable. In a reported series, about 6 % of patients died, about 32 % survived but were left dependent, about 32% had some deficits but were independent, and about 30% recovered completely. Initial clinical features are not predictive of outcome and a recent case series found conventional MRI findings were not prognostic but the prognostic role of diffusion-weighted imaging is still unclear 3,4,8.
In conclusion, CPM and EPM are the same disease, sharing the same pathology, associations, and time course but differing in clinical manifestations due to differences in the affected structures. Both diseases have lesions that are strikingly symmetrical.