This short video offers breathtaking views from the peak of Mt. Bandilaan, the highest peak and dead center of Siquijor island. Actually, this is the first mountain I scaled and it's pretty easy: there are narrow trails leading to the peak of the mountain. Mr. Johnson Siangco, my kindly guide and habal-habal driver, points to the six towns of Siquijor as I point my video cameras on those towns. The six towns of Siquijor are Siquijor, Lazi, Maria, Enrique Villanueva, San Juan, and Larena. I stayed for five days and four nights in Siquijor island. I would say that Siquijor is one of the loveliest places in the Philippines. Actually, exploring the beauty of the island, one easily forgets the Mangkukulam ;)
Thursday, September 30, 2010
Wednesday, September 29, 2010
Kristong Hari's Message to P-Noy!
Mr. Lauro Gonzales, aka, Kristong Hari, has been for a long time trying to seek an audience with Philippine Presidents (from Marcos to Arroyo), but could not get past the Presidential Security Guards in Malacanang Palace. The Palace guards would not let him near the presidential gate, much less inside the palace grounds.
Now Kristong Hari asked me to film this video message to the newly-elected President Noynoy Aquino. He was possessed here by the Santo Nino (Child Jesus) so his voice was small, resembling that of a small child. Of course, I would not know if he is only acting here or truly possessed by the Santo Nino. I do not want to judge him. If he believes he is God, then I cannot do anything about it.
Kristong Hari is very serious in his attempts to make contacts with global leaders because he claimed he can be the one to solve all global problems. Some would say that Kristong Hari has delusions of grandeur and even a lunatic. But I found him sincere in his belief that he is God.
This short clip is shot in front of Quiapo Church where Kristong Hari and his followers congregate every Friday to bless people and ask for their donations. To those who help him, he promises eternal life. Those who do not will perish in the fires of hell. Well, I didn't want to go to hell, so I decided to give him with some amount of money every Friday. He appreciates that I take the time to listen to him, unlike the many others who malign him and his followers, and even label them as lunatics.
I think that Kristong Hari is a sincere and genuinely kind man, although I do not cater to his claim that he is the incarnation of Jesus Christ. But then it touched my heart that he wanted me to become one of his saints. Although it was an honor, I respectfully declined his offer as I am not holy and perfect. It just pleases me to document a strange and fascinating man like him--not to judge him but to understand him better.
Now Kristong Hari asked me to film this video message to the newly-elected President Noynoy Aquino. He was possessed here by the Santo Nino (Child Jesus) so his voice was small, resembling that of a small child. Of course, I would not know if he is only acting here or truly possessed by the Santo Nino. I do not want to judge him. If he believes he is God, then I cannot do anything about it.
Kristong Hari is very serious in his attempts to make contacts with global leaders because he claimed he can be the one to solve all global problems. Some would say that Kristong Hari has delusions of grandeur and even a lunatic. But I found him sincere in his belief that he is God.
This short clip is shot in front of Quiapo Church where Kristong Hari and his followers congregate every Friday to bless people and ask for their donations. To those who help him, he promises eternal life. Those who do not will perish in the fires of hell. Well, I didn't want to go to hell, so I decided to give him with some amount of money every Friday. He appreciates that I take the time to listen to him, unlike the many others who malign him and his followers, and even label them as lunatics.
I think that Kristong Hari is a sincere and genuinely kind man, although I do not cater to his claim that he is the incarnation of Jesus Christ. But then it touched my heart that he wanted me to become one of his saints. Although it was an honor, I respectfully declined his offer as I am not holy and perfect. It just pleases me to document a strange and fascinating man like him--not to judge him but to understand him better.
Tuesday, September 28, 2010
Neurovascular compression syndrome of VII-VIII cranial nerves



Findings
High resolution T2 images at the level of the internal auditory meatus demonstrate the facial and vestibulocochlear cranial nerves entering the internal auditory meatus. The facial nerve lies anterior while the eighth cranial nerves courses posteriorly. With the left side used for reference, a tortuous basilar artery is seen posteriorly displacing the normal course of the right vestibulocochlear/facial nerve complex. The presumed point of symptomatic compression is encountered posteriorly as the nerve complex “bends” over posterior aspect of the internal auditory meatus. Although sometimes seen in asymptomatic individuals, when findings are viewed in the appropriate clinical setting, NVCS should be raised as a diagnostic possibility.
Diagnosis: Dolichoectasia of the basilar artery causing right sided sensorineural hearing loss
Hearing loss can be characterized as either conductive or sensorineural based on clinical exam and audiometry. Conductive hearing loss involves an abnormality of the external auditory canal to the oval window and is best evaluated with high resolution CT as it is able to display the external auditory canal and middle ear structures, particularly the ossicles. Sensorineural deafness implies an abnormality of the inner ear, vestibulocochlear nerve, or its central components which are best evaluated with MRI.
Neurovascular compression syndrome (NVCS) refers to a group of disorders in which an aberrant or tortuous vessel causes nerve compression with subsequent hyperexcitation and neuropathy. Vascular compression syndrome has been described as a causative etiology for cranial nerves III, V, VII, VIII, and IX. Controversy exists, however, because of the normal intimate apposition of nerves and vasculature around the brainstem and the frequency with which it is seen in asymptomatic patients.
Vestibulocochlear NVCS is symptomatic vascular compression of cranial nerve VIII. Clinical symptoms are often non-specific including tinnitus, vertigo, and sensineural hearing loss. A recent article in the American Journal of Neuroradiology failed to reliably determine neurovascular compression as a cause of tinnitus although some authors maintain it may still be considered when presenting with so called "typewriter" tinnitus. In decreasing order of frequency, vessels indicated in NVCS include the anterior inferior cerebellar artery, posterior inferior cerebellar artery, and vertebral artery.
The following MRI classification system for neurovascular compression has been proposed to aid in surgical planning.
- Type I: Point compression where a limited segment of the nerve is in contact with the vessel.
- Type II: Longitudinal compression in which the nerve and vessel traverse parallel to each other.
- Type III: A vascular loop encircling the neve.
- Type IV: The nerve contour is deformed and/or thinned.
Definitive treatment involves retromastoid craniectomy and microvascular decompression in which a small synthetic sponge is interposed between the offending vascular structure and nerve.
Monday, September 27, 2010
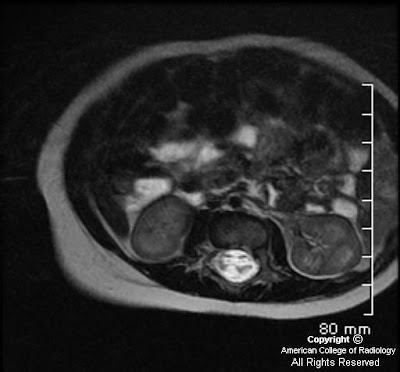
Long standing Portal hypertension-CT
Shrunken liver with nodular outline and relative enlargement of the caudate lobe. These are consistent with chronic liver disease. GB is contracted with thickened, possibly edematous walls. IHBR dilatation in this possibly indicates associated portal biliopathy. Calcification in relation to anatomical site of the main portal vein, porta hepatis and spleinc vein. Spleen is enlarged. Calcification is also noted in the splenic parenchyma which is seen extend along the vascular branches. Calcification in the portal venous system is known to occur in the long standing portal hypertension. Collateral/tortousity noted in perisplenic region and lienorenal region. Collaterals are alos noted along the body wall. Gross ascites. Wall thickening in the GE junction which may indicate varices. Stomach wall is also thickened.
Kristong Hari: A Short Video Preview
This short video clip is part of the documentary movie I am currently filming on the life story of Mr. Lauro Gonzales, a.k.a. Kristong Hari, the man who believes he is Jesus Christ. In this short clip, you can see Kristong Hari's devotees praying and worshipping him as the true living Jesus Christ. This was filmed in Plaza Miranda, in front of the Quiapo Church, in Manila.The whole movie will be coming soon! ;)
My friend Sidney Snoeck is currently featuring Kristong Hari in an amazing photo series here. We have been following Kristong Hari for sometime now, although not as faithfuls! But then, Kristong Hari wanted us to become his saints: me as St. Peter, and Sidney as St. Jude!
Tuber cinereum hamartoma-MRI
A hypothalamic or tuber cinereum hamartoma is benign non neoplastic heterotrophic lesion in the brain that typically occurs about the hypothalamus. The tuber cinereum is a part of the hypothalamus located between the mamillary bodies and the optic chiasm. Thought to arise from anomalous neural migration between 35 and 40 days in utero (time of hypothalamic formation). This is isointense to gray matter on T1 weighted images and hyperintense on T2 and FLAIR images. There was no post gadolinium enhacement. This is 28year old male.
Thursday, September 23, 2010
Radiology Residency
Road versus destination.This possibly happens to all of us sometime or the other. I always cross DND to reach my hospital from home and am usually late, never really noticed the beautiful river below and what all you could see while on the road and my main concern was to avoid getting late and honking. Today with the common wealth causing this crazy jam at the ashram crossing, realised that there is nothing i could do about it and started to see around and saw the our river yamuna with these rains is actually looking amazingly beautiful and that you can see the lotus temple at the distance from the middle of the road and huge building of barakambha at the distance. May be this is true for our residencies as well, most of us while doing our post graduation are more concerned about the destination, that we fail to enjoy the time we have at that time to learn without actually thinking of the returns and ways to increase business. Residency is one of the best times of our education as although there are pressures of exam, on call duties and struggle to understand more and more things which apparently appear simple to the seniors around, still we are at the peak of our knowledge quest and skill acquistion.
Filar cyst


Findings
Figure 1: Axial T2-weighted image demonstrates a cystic structure in the filum terminale.
Figure 2 and Figure 3: Coronal T2-weighted images demonstrate a cystic structure in the proximal filum terminale.
Diagnosis: Filar cyst
The human spinal cord develops through three distinct stages: neurulation, canalization, and retrogressive differentiation. The conus medullaris, filum terminale, and cauda equine are mainly developed and formed in the retrogressive differentiation stage as the caudal cell mass regresses.
Cystic structures within the distal spinal cord, conus medullaris, and filum terminale are commonly seen on routine lumbosacral spine sonography in the neonates. These patients often present with abnormal laboratory values and/or external body features that are suggestive of underlying spinal dysraphism or neural tube defects. The diagnostic consideration of a cystic lesion in this region includes: syrinx, neoplasm (ependymoma or astrocytoma), persistent ventriculus terminalis in the conus medullaris, and filar cyst in the filum terminale of the cord.
Filar cysts are a relatively common entity in the neonates usually detected on screening lumbosacral sonograms. However, it has not been extensively reported in the literature. It is considered a normal variant when found as an isolated finding. The exact etiology of a filar cyst has not been reported. Literature has suggested that filar cysts are developmentally similar to the septum pellucidum and ventriculus terminalis, which can regress with age. On ultrasound, it is usually describes as an anechoic, cystic structure completely contained within the filum terminale. MRI of the lumbosacral spine can be obtained in cases that are questionable on ultrasound. Filar cyst follows the typical characteristic of a simple cyst in all sequences of an MR study. Ventriculus terminalis is a normal developmental variant described as a nonenhancing dilation of the ependyma-lined central canal at the level of the conus medullaris. Persistent ventriculus terminalis deserves special attention such that it is often used interchangeably with filar cyst in the literature, in the setting of cystic lesions seen in the distal lumbar spinal cord proximal to the conus medullaris. A cystic lesion in the absence of a solid component makes a neoplastic process less likely. A syrinx isolated to the distal spinal cord is also less common as it usually has a superior extension.
Treatment options are primarily based on patient's symptomatology. In asymptomatic neonates/infants, no further imaging is needed.
Wednesday, September 22, 2010
Melanotic Neuroectodermal Tumor of Infancy (MNTI)
Findings
Large mass involving left side of face with invasion, mass effect, and extensive bony involvement. The mass does not appear to cross the midline. Enhancing focus on MR adjacent to the superior aspect of the falx and superior sagittal sinus. FDG-avid spine lesions.
Diagnosis: Pathology-proven melanotic neuroectodermal tumor of infancy (MNTI)
Discussion
MNTI is a rare osteolytic, pigmented neoplasm that typically affects the head and neck, predominantly the maxilla, of infants. It is typically considered a benign lesion, with only a few reported cases of metastatic disease reported in the literature. It usually presents in the first year of life. It may appear as a rapidly expanding, non-ulcerated, lightly pigmented, blue or black lesion on the anterior aspect of the maxilla. It may extend intraorally, cause bone destruction and dislodgement of teeth.
MNTI is considered to be of neural crest origin, and some patients will high urinary excretion of vanillylmandelic acid (VMA). The tumor is typically non-encapsulated, showing local invasion of bone. The histologic appearance is similar to other cells of neural crest origin, demonstrating small, round blue cells, as well as containing a moderately vascular fibrous background. Part of the lesion may contain large polygonal cells arranged in sheets that contain melanin. Immunohistochemistry and electron microscopy can aid in the final diagnosis. The few reported cases of malignant disease have noted increased numbers of mitoses per high-powered field.
Conventional radiography may demonstrate a well-circumscribed or ill-defined radiolucency, with destruction of bone as the lesion progresses. CT can delineate the extent of soft tissue involvement and osteolysis. Contrast-enhanced MRI can demonstrate soft tissue tumors with nonenhancing, heterogeneous tissue density and can also demonstrate osseous involvement. There may be foci of T1-hyper/T2-hypointensity secondary to melanin.
Surgical excision with partial maxillectomy and 5 mm margins are typically curative, with 10-15% recurrence rates. There are no standards of care for malignant disease.
Initial biopsy of this patient's facial lesion demonstrated a high mitotic index. After 2 surgical excisions and recurrence, the patient developed intracranial and spinal column metastases. The patient underwent multiple cycles of radiotherapy and chemotherapy. The intracranial lesion was never biopsied due to the precarious location, however it has regressed, and there appears to be a slight interval decrease in size of the soft tissue component of the maxillary lesion.
Tuesday, September 21, 2010
Telestroke
According Steven R. Levine and Mark Gorman, MD From the Center for Stroke Research & Henry Ford Stroke Program in Stroke. 1999;30:464-469; Time is of the essence for effective intervention in acute ischemic stroke. They emphasize that computer-based technology can now be used to integrate electronic medical information, clinical assessment tools, neuroradiology, laboratory data, and clinical pathways to bring state-of-the-art expert stroke care to underserved areas.
Further reading and reference
Further reading and reference
"Telestroke" The Application of Telemedicine for Stroke
Hypertrophic cranial pachymeningitis-MRI
Hypertrophic cranial pachymeningitis is a rare chronic fibrosing inflammatory disease characterized by marked diffuse thickening of the cranial dura mater that causes progressive neurological deficits. Chronic headache and cranial neuropathy are the common clinical manifestations of patients with hypertrophic cranial pachymeningitis. Gadolinium enhanced T1WI, coronal sequence, reveals markedly thickened and enhancing falx and tentorium cerebelli. This is a 35yr old female with chronic headache.
Saturday, September 18, 2010
Hematometra with hematosalpinx-MRI
This is 13 year old who had abdominal pain and had not yet achieved menarche. MRI revealed blood distended in the uterine cavity and bilateral hematosalpinx. Right sided rudimentary horn was also suspected.
Friday, September 17, 2010
LV Contrast for R/O Thrombus
This one is shared from the youtube and for all the residents this is how ultrasound contrast agent work for cardiovascular imaging.
Thursday, September 16, 2010
Does the choice of MRI machine matter?
"This is about an article on Kevin MD in which a patient underwent MRI cervical spine for neck pain and was reported normal. Imaging was substandard and physician wanted another repeat MRI. However, insurance company refused as MRI was just done a week back. Patient was admitted and repeat study revealed cervical herniated disk."
- My question in India in lot of places MRI are done in permanent magnet at about 0.3T strength and pathologies are often missed. Are they justified?
- As a Reporting Radiologist will you write on such reports suboptimal for reporting?
- What is the way out, for radiologists as if you are on payroll, you cannot possibly write suboptimal on each study and get paid for it as well. What if the patient sues the first radiologist for missed diagnosis, does he have the defense opf suboptimal machine and for that matter how do you define a suboptimal machine?
Funnel chest (pectus excavatum)-CT
Funnel chest (pectus excavatum), the sternum is depressed so that the ribs on each side protrude anteriorly more than the sternum itself. Posteroanterior radiography also depicts parasternal soft tissues of the anterior chest wall as an area of increased density in the inferomedial portion of the right hemithorax. The severity of the deformity is best quantified with CT.
The “pectus index” can be derived by dividing the transverse diameter of the chest by the anteroposterior diameter. Normal value of this index to be 2.56 (±0.35 SD) and suggested that a pectus index greater than 3.25 necessitated surgical correction.
The “pectus index” can be derived by dividing the transverse diameter of the chest by the anteroposterior diameter. Normal value of this index to be 2.56 (±0.35 SD) and suggested that a pectus index greater than 3.25 necessitated surgical correction.
Wernicke’s encephalopathy
Findings
There is increased T2 signal and diffusion restriction in the thalami bilaterally. There is no contrast enhancement.
Diagnosis: Wernicke’s encephalopathy
Discussion
Wernicke's encephalopathy occurs with vitamin B1 (thiamine) deficiency. It is associated with malnutrition and is commonly seen in alcoholics. Wernicke's encephalopathy manifests itself as memory loss, ataxia and oculomotor dysfunction. Thiamine plays a vital role as a cofactor for several enzymes involved in carbohydrate metabolism. Without thiamine, the energy requirements of neuronal cells are not met resulting in cell death and neurologic dysfunction.
Wernicke's encephalopathy is reversible and if suspected, treatment should begin promptly. Parenteral thiamine should be administered promptly. The thiamine should be given prior to any glucose infusion. The addition of glucose in a thiamine deficient patient will exacerbate the encephalopathy. Patient's with thiamine deficiency are also likely to be hypomagnesemic and parenteral magnesium sulfate should also be administered.
Radiologic overview of the diagnosis
Wernicke's encephalopathy manifests itself as increased T2 signal in the medial thalami, hypothalamus and periaqueductal grey matter. There is associated diffusion restriction in affected areas. In chronic cases, there is atrophy of the mamillary bodies. The sensitivity of MR to diagnose Wernicke's is estimated at approximately 50% so the lack of these imaging findings, do not exclude the diagnosis of Wernicke's encephalopathy. CT is even worse than MR in the diagnosis of Wernicke's and should be used to rule out an acute intracranial process. Alcoholic induced Wernicke's will manifest the same above findings, but will also show superior vermian atrophy.
In this case, there is increased T2 signal and diffusion restriction in the medial thalami bilaterally. There is no contrast enhancement. The patient has lymphoma and a chronic history of vomiting. With this history, Wernicke's encephalopathy was thought to be the cause of the patient's altered mental status. The lack of contrast enhancement makes the diagnosis of lymphoma highly unlikely.
Solitary Fibrous Tumour of the Orbit-CT
SFT might be included in the differential diagnosis of soft tissue masses in the orbit, if one sees a markedly enhancing mass showing the similar characteristics to those of the internal carotid artery on postcontrast CT or MR images. Since the first report by Klemperer and Rabin1 in 1931 as a primary spindle-cell tumor of the pleura, solitary fibrous tumor (SFT) has been recognized as a distinctive, though rare, pathologic entity that most commonly arises from the pleura and peritoneum.
Wednesday, September 15, 2010
Anterior communicating artery aneurysm
Findings
The head CT without contrast shows a region of hyper density along the anterior falx along the course of the anterior cerebral artery concerning for acute blood products. CT angiogram shows an anterior communicating artery aneurysm that splays both anterior cerebral arteries and points anteriorly No definite blood products within the suprasellar cistern are seen. There is no intraventricular hemorrhage.
Diagnosis: Anterior communicating artery (ACom) aneurysm (unruptured)
Key points
Aneurysm development and rupture risk reflect complex combination of inherited susceptibility and acquired mechanically-mediated vessel wall stresses4."
Associated with connective tissue disorders such as fibromuscular dysplasia, Ehlers-Danlos syndrome (type IV), ADPCKD
Familial intracranial aneurysms: Occur in clusters of 1st degree relatives
Location: 90% arise from circle of Willis
- 90% anterior circulation (Acom and internal carotid-com most common sites)
- 10 % posterior (Basilar artery bifurcation, PICA most common)
- 1-3% misc sites distal to COW (often traumatic, mycotic, oncotic)
Risk of rupture:
- Increased risk of rupture:
- Size
- Multilobed
- Apical "bleb"
- Length: neck aspect ratio >1.6
Giant aneurysms (>2.5cm) present both the risk of rupture and symptoms related to mass effect
15-20 % multiple
Estimated risk of rupture: 1-2% year cumulative for unruptured aneurysms
Demographics:
- F>M (especially with multiple aneurysms)
- Incidence: 1/100000 (<35yo); 44/100000 (>65yo)
Treatment: Cost-effective strategy for unruptured aneurysms
- Endovascular treatment was most cost effective for anterior circulation aneurysms 7-25 mm in size
- No treatment was most cost-effective for anterior circulation aneurysms < 7mm
- Surgical treatment was most cost effective for anterior circulation aneurysms > 25m
- Endovascular coiling has been accepted as effective treatment, though controversy still exists between surgical and endovascular therapy.
Long-term (10yr) followup of 1036 coiled aneurysms required retreatment in 7% and rebleeding in 0.5%
Tuesday, September 14, 2010
Papillary cystic and solid tumour of the pancreas-CT
The Papillary cystic and solid tumour of the pancreas (PCSTP) is an unusual low-malignant epithelial tumour, which mostly affects young females with a mean age 25 years. It has also been referred to as a solid-cystic epithelial tumour, solid-pseudopapillary tumour or papillary-cystic tumour. Typically, on CT scan PCSTP tumours appear as sharply circumscribed, well-encapsulated, heterogeneous and hypodense lesions. This is a 37 year female with histologically proven case of PCSTP.
Postictal Imaging Findings
46-year-old male presented to the emergency room after a first seizure. He has no significant or contributory past medical history.
Follow-up FLAIR imaging obtained approximately 5 weeks later.
Findings
Figure 1 and Figure 2: FLAIR and DWI images show abnormal increased signal in the left temporal lobe. The right temporal lobe is questionably involved. The differential diagnosis for these findings included, but is not limited to, neoplasm, infection, and postictal changes.
Figure 3: Follow-up FLAIR imaging obtained approximately 5 weeks later demonstrates resolution of these findings, consistent with postictal change.
Diagnosis: Postictal Imaging Findings
A seizure is "a sudden alteration of the CNS resulting from a paroxysmal high frequency or synchronous low frequency, high voltage electrical discharge". Imaging (CT or MRI) is indicated in cases of:
- New onset of seizure activity
- Change in pattern of previous seizure pattern
- Patients with focal neurological defects or altered mental status
- Prolonged postictal state, especially if associated with neurological defects
Following seizure activity, imaging is used to identify an underlying etiology. Differential possibilities include structural/anatomical abnormalities, space-occupying masses (primary or secondary brain neoplasms, abscesses), cerebrovascular accidents, transient ischemic attacks, hemorrhage, infectious processes (meningitis, encephalitis) venous thrombosis, and vasculitis. If performed shortly after the ictal event, CT and MR imaging may demonstrate findings that are secondary to the physiological mechanisms related to the seizure itself. These findings are most likely to occur following status epilepticus.
The mechanism and pathophysiology of these findings are unknown. Some theories are that the findings occur as a result of breakdown of the blood brain barrier. This results in transient focal brain edema, accounting for various imaging findings. Other theories propose arteriovenous shunting of blood during seizure activity that results in accumulation of toxic metabolites, ischemia, and acidosis. Most theories implicate ischemia and transient cytotoxic edema as the cause of brain changes.
Imaging findings are nonspecific and can overlap with those seen in other disease entities such as infarction/ischemia, venous thrombosis, vasculitis, infection, neoplasm, arterial thromboembolism and metabolic encephalopathy. History, presenting signs and symptoms, follow-up imaging and other relevant laboratory data can further narrow the differential diagnosis.
On CT, possible postictal imaging findings include:
- effacement of adjacent cortical sulci
- focal gyral edema
- decreased gyral attenuation
- mild to moderate gyral enhancement on contrast-enhanced images
On MRI, possible findings include:
- increased signal on T2WI (most common in the frontal and parietal lobes but also seen in the temporal and occipital lobes as well as other regions in the brain such as the hippocampus)
- corresponding hypointensity on T1WI
- abnormal contrast enhancement
- diffusion restriction and reduced ADC
- gyral swelling with effacement of adjacent sulci
Bilateral involvement is more common than unilateral. Lesions usually overlap arterial and watershed territories. In addition, lesions are usually in the cortex or subcortical white matter and spare the basal ganglia. Studies have shown leptomeningeal enhancement on post-contrast MRI. Follow-up imaging reveals complete or near-complete resolution of these findings.
It is important to recognize the various imaging findings that can be seen in the postictal period to avoid unnecessary biopsy and further workup such as angiography and biopsy. The postictal imaging appearance can be confused with other entities such as neoplasm, infection and infarction. The amount of time until resolution of these transient imaging findings is unclear. Studies have shown resolution of postictal changes in as low as 5 days. However, the majority of cases resolve over weeks - months. Patients should be re-imaged to confirm the transient nature of abnormal MR findings, usually within 4 - 6 weeks. It is important for patients to be re-imaged only after a seizure-free interval.
Subscribe to:
Posts (Atom)

























