Findings
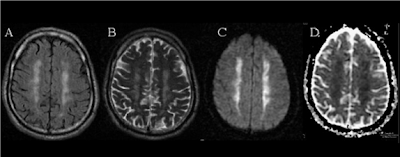
Figure A: Axial FLAIR shows bilateral symmetric high intensity signal in the centrum semiovale.
Figure B: Axial T2 weighted shows bilateral symmetric high intensity signal in the same areas.
Figure C: Axial DWI shows bilateral symmetric restricted diffusion in the same areas.
Figure D: Axial ADC shows restricted diffusion in the same areas.
Diagnosis: Man-in-the-barrel syndrome (MIBS)
The term man-in-the-barrel syndrome (MIBS) was coined by Sage in 1983 to describe the association of several clinical features which often occur together in patients with disproportionate weakness of both arms (especially proximally) and relatively normal mobility of face and legs, as though the trunk of the patient is stuck in a barrel. Since then, there have been multiple case reports in the literature describing observed MIBS believed to be caused by severe systemic hypotension related to emergent CABG , hemorrhagic shock , and severe anaphylaxis. Bilateral ACA-MCA watershed infarcts may be a common factor in all of these clinical scenarios. However, there have also been several reports of processes other than watershed infarcts with a clinical presentation similar to MIBS, including motor neuron diseases, pontine myelinolysis, glioma and vertebral artery dissection.
The dominant mechanistic theory explaining MIBS is that of bilateral symmetric watershed infarction in the region perfused by medullary arteries from the superficial pial plexus and deep penetrating arteries from the basal cerebral arteries, which has been known for at least 40 years. A related neurological entity, brachial diplegia due to pyramidal tract involvement was first described by Mohr in 1969. Although there have been several papers decribing the CT or MR features of watershed infarcts between the territories perfused by MCA and ACA, especially the corona radiata and centrum semiovale, it is unclear exactly which focal neural pathway is disrupted that directly leads to the clinical presentation of MIBS. It is postulated that there is a threshold for the amount of confluently affected paraventricular white matter above which MIBS may become manifest.
Despite the uncertainties mentioned above, MIBS remains a fascinating clinical phenomenon. Further research will hopefully better define this entity.
No comments:
Post a Comment