

Prostatic carcinoma is the most common malignancy affecting males older than 50 yrs. The combination of serum PSA levels, clinical TNM staging and histopathologic Gleason scoring dictates the course of treatment. Nodal disease is classified as local lymph node involvement within the true pelvis, whereas metastatic lymph node disease is involvement outside the true pelvis. Usually internal iliac and obturator lymph nodes are involved first.
International Staging System for Prostate Cance
I (T1, N0, M0)
Organ confined, clinically and radiologically inapparent.
II (T2, N0, M0)
Organ confined, clinically or radiologically apparent
T2A : ≤ 50 % of single lobe involved.
T2B : ≥ 50% of single lobe involved.
T2C : both lobes involved.
III (T3, N0, M0)
Extracapsular extension or seminal vesicle invasion.
T3A : extracapsular extension.
T3B : seminal vesicle invasion.
IV (N1-2)
Local or regional adenopathy.
N1: microscopic nodal metastases.
N2 : macroscopic nodal metastases.
V (T4 or N3 or M1-2)
Distant metastases.
T4 : bladder, external sphincter or rectal invasion.
N3 : extraregional nodal metastases
M1 : elevated alkaline phosphatase elevation.
M2 : distant visceral or bony metastases
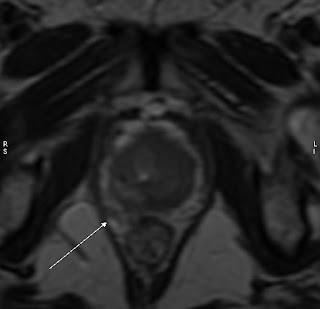
CT is not very reliable in determining tumour extension through the prostate capsule but in determining abdominal and pelvic lymph nodes involvement. On MRI, T1WI, the homogeneity of prostate can make tumour detection difficult. The normal peripheral zone T2 hyperintensity is replaced with low signal from the tumour. Seminal vesical involvement is also discernible on MRI with replacement of normally T2 hyperintense tumour with hypointense tumour.
International Staging System for Prostate Cance
I (T1, N0, M0)
Organ confined, clinically and radiologically inapparent.
II (T2, N0, M0)
Organ confined, clinically or radiologically apparent
T2A : ≤ 50 % of single lobe involved.
T2B : ≥ 50% of single lobe involved.
T2C : both lobes involved.
III (T3, N0, M0)
Extracapsular extension or seminal vesicle invasion.
T3A : extracapsular extension.
T3B : seminal vesicle invasion.
IV (N1-2)
Local or regional adenopathy.
N1: microscopic nodal metastases.
N2 : macroscopic nodal metastases.
V (T4 or N3 or M1-2)
Distant metastases.
T4 : bladder, external sphincter or rectal invasion.
N3 : extraregional nodal metastases
M1 : elevated alkaline phosphatase elevation.
M2 : distant visceral or bony metastases
CT is not very reliable in determining tumour extension through the prostate capsule but in determining abdominal and pelvic lymph nodes involvement. On MRI, T1WI, the homogeneity of prostate can make tumour detection difficult. The normal peripheral zone T2 hyperintensity is replaced with low signal from the tumour. Seminal vesical involvement is also discernible on MRI with replacement of normally T2 hyperintense tumour with hypointense tumour.
No comments:
Post a Comment